The burning question: Does tobacco have a future in a healthy world?
Few dispute the fact that smoking tobacco is linked to lung cancer and other health issues. It takes a few decades but eventually smoking will kill half of its habitual users, estimated globally to be 7.7 million deaths in 20191. In the ideal world, smokers would heed these statistics, but the powerful addictive effect of nicotine ensures that progress towards that goal is frustratingly slow. Indeed, despite a small decline in the rate of smoking, recent global population growth has actually led to a small increase in the total number of smokers.

What are ECs and HTPs?
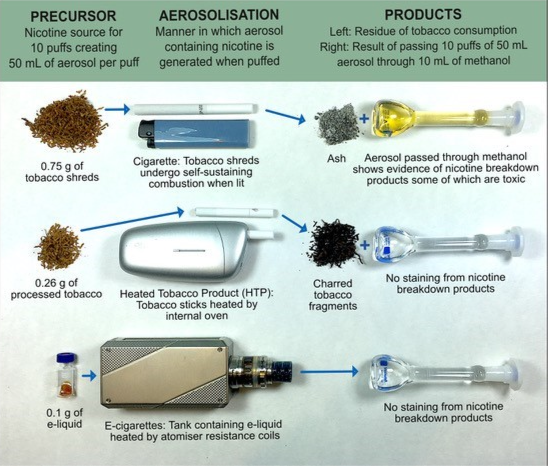
Recognising that quitting smoking is very challenging, and that nicotine itself is not the main toxic substance in cigarettes, devices that simulate the act of smoking have become popular by offering users alternative ways to satisfy their need for nicotine. These devices can deliver adequate amounts of nicotine but emit much lower concentrations of the harmful chemicals created by conventional cigarettes. Two sources of inhalable nicotine other than combustible cigarettes are of interest here:
E-cigarettes (ECs) contain purified nicotine (with or without flavours and other additives) dissolved in a carrier liquid which is heated and converted into a breathable aerosol (vaping). Such heated liquid devices are now used by 3.6 million people in the UK, mostly ex-smokers2.
Heated tobacco products (HTPs) do not generally involve liquids; instead, they heat processed tobacco to a temperature sufficient to release nicotine. These products are sometimes termed “Heat not Burn” by the tobacco industry as heating is said not to reach the point of combustion when, it is claimed, most of the highly toxic compounds in tobacco smoke are formed. These are sometimes considered to be a form of vaping.
Establishing a basis for comparison
We know from surveys of current smokers that reducing the risks to health is their main motivation for quitting, yet these same surveys invariably reflect considerable confusion on the risks of vaping as an alternative to smoking2. Subsequently, research at the University St Andrews recognised the need to establish a basis for comparing health impacts. Because health risk is normally related to exposure, researchers have focused on the relative exposures to cancer-causing chemicals (carcinogens) from combustible cigarettes, ECs and HTPs.

The most accurate approach to assessing the cancer risks of smoking is to count the casualties, that is to compile the clinical symptoms and deaths over the several decades necessary for all the cancer-related health effects to become manifest. Because ECs and HTPs are recent innovations, adopting this approach means waiting a few decades before firming up policies and regulation of these products in the interests of public health. Obviously, waiting that long is not the ideal strategy. Instead, Dr Ed Stephens of the School of Earth and Environmental Sciences looked to find measures of exposure that influence long-term health trajectories.
Dr Stephens’ work focused on the quantities of carcinogenic chemicals present in the aerosols that smokers and vapers inhale. Other scientists approach the same issue by measuring biomarkers reflecting the user’s biological reactions to exposure to these aerosols, or by observing the effects in similarly exposed cell cultures or animals. There is a broad consensus among these diverse approaches that the reduced exposure to carcinogens from most ECs and HTPs results in reduced indications of cancer risk compared with smoking.
Estimating the risks (click to expand)
While decades of research have provided us with very detailed knowledge of what is present in tobacco smoke, we are presently less certain that we know all the hazardous components of e-cigarettes. Not all chemicals are equally carcinogenic, some are much stronger carcinogens than others in terms of their potency for causing cancer. Whereas there is a lot of information on the harmful properties of chemicals we ingest in food and drink, there is much less information on the chemicals we inhale in the air and through smoking or vaping products. These and other uncertainties mean that we are unable yet to make accurate estimates of the cancer risks (or any other disease) of vaping products. However, useful information can be obtained by summing the concentration of each carcinogen weighted by its cancer potency (where available) for all identified components, rather than the common practice of considering each carcinogen separately. This sum of individual exposures (E) reflects the cocktail of cancer-causing chemicals in the whole aerosol and serves as a useful ballpark guide to cancer risk.
Dr Stephens’ approach enables the comparison of nicotine-delivering vaping products to traditional combustible cigarettes by estimating these E values from inhaling identical amounts of aerosol emitted by different products.
Using a simple exposure ratio (ER) where ERaerosol = Eaerosol/Ecigarette smoke to compare a given nicotine-delivering aerosol with cigarette smoke under identical conditions, we find ER=1 for combustible cigarettes while other products are expressed as order of magnitude differences from 1, i.e. deviations by powers of 10. In this way, an ER value of 1 (100) would represent an exposure equivalent to that of smoking, whereas ER values of 0.1 (10-1) and 0.01 (10-2) represent exposures of one tenth and one hundredth of smoking, respectively. As there is roughly a 100,000-fold (105) range in ER between tobacco smoke and smoke-free air, our use of powers of 10 provides useful discrimination between nicotine aerosols while reflecting uncertainties in the model. If hitherto undetected carcinogens are discovered in any of these aerosols, their concentrations would need to be very high to cause a 10-fold increase ER. Similarly filling the gaps in cancer potencies would require extremely carcinogenic values to change the order of magnitude of ER. Thus, radical revisions of the ERs presented below are considered unlikely but not impossible.
ECs (e-cigarettes that heat liquid nicotine without tobacco) have a very wide range of ER values extending from 0.0001 to 1, from that of a medically prescribed nicotine inhalator to that of smoking. The ER values that fall in the range 0.01 to 1 are generally associated with excessive heating of the device beyond its recommended limits causing chemical breakdown of liquid components to form carcinogens. Some modern devices are now designed to prevent this happening. More typically, the ER values of EC emissions are much lower, rarely exceeding 0.01 and most measured aerosols have ERs less than 0.001.
HTPs (heated tobacco products) have ER values around 0.1, suggesting a 10-fold reduction in the exposure to carcinogens and a likely reduction in cancer risk of the same order.
The global impact

Proxies of health impact are influencing the global effort to reduce the toll of smoking on public health. The UK Government, through Public Health England, has pioneered a sometimes-controversial policy to promote e-cigarettes as aids in smoking cessation, citing evidence described above among others.
Philip Morris International, maker of the world’s best-selling cigarette brand, Marlboro, with an annual revenue in 2020 of $76 billion, has developed a novel HTP called iQOS. Other leading tobacco companies have developed, or are in the process of also developing, HTPs of their own. In July 2020, Dr Stephens’ research was used as evidence in the approval of the iQOS as a “modified risk tobacco product” by the Food & Drug Administration (FDA), the body which regulates tobacco products in the US. The FDA stated that the iQOS range was “expected to benefit the health of the [US] population as a whole”. It is important to stress that this does not mean these products are safe, however.
Does tobacco have a future in a healthy world? The tobacco industry certainly thinks so. They have invested billions of dollars in creating and marketing their novel heated tobacco products. The FDA approval of their HTP products led Philip Morris to release a statement in July 2020 which announced a radical change to the company’s long-term business strategy away from cigarettes, replacing them with smoke-free, non-combustible products. They stated “… we have committed to stop selling cigarettes as soon as possible. Our ambition is to secure a smoke-free future for all”3.
Is a healthier world without tobacco possible?
The research at St Andrews has shown that exposure to carcinogens from HTPs may be reduced on average by as much as 10-fold, but exposure to 10% of the colossal dangers of smoking is still a considerable risk. Electronic cigarettes do not use tobacco and their aerosols tend to reduce current ER estimates for cancer by 100-fold or more when used at low power settings.

Dr Stephens states, “alternatives to combustible tobacco are rapidly evolving and, if they can decrease the exposure to harmful chemicals still further while providing users with a nicotine source as satisfying as smoking, the journey to a smoke-free future becomes a realisable ambition. Guidance on this journey will require research into better risk models based on comprehensive data on emitted compounds and their inhalation effects, applied not just to cancer but to all the diseases associated with smoking and vaping.
The route to a healthier world without smoke and perhaps without tobacco is not without dangers of its own. Possibly the most hazardous is the risk of introducing nicotine to minors, through new products that are enticingly flavoured and attractively marketed. However, regulation and education can help mitigate these dangers, increasing the likelihood that the journey out of the smoke arrives at a much better destination. As we strive towards freedom from tobacco smoke, perhaps we can dare chart further routes to an even healthier world without nicotine.”